Why does a midwife with 3 daughters care about infant male circumcision?
When I was a young nurse, it was part of my job to assist with circumcisions of healthy baby boys. My responsibilities went like this: gather all the newly born babies scheduled for circumcision that morning (usually on the day of discharge from the hospital) and bring them to the nursery. Prepare the procedure room for the surgeries by setting up the restraint board, the surgical supplies, and the physician's clamp of choice: either Mogen, Gomco, or Plastibell. Then comes the first part of what haunts my dreams...I then tied the babies down on the restraint board. The babies obviously did not like being tied down, especially since that they had been curled up in a ball for their entire existence. Parents were commonly told "He cried when we put the straps on him more than for the actual circumcision!" Even if that were true, why is that less of a concern?
Once the physician arrived and began the surgery, it was my job to attempt to comfort the babies. Or at least make them quieter & seemingly in less pain. I would dip my finger in sugar water and encourage them to suckle. I would put my lips near to their ear and say "ssshhhhhhh" or speak sweetly to them. I would try to comfort them as best as I could. Well over a hundred baby boys had their penises cut to the sound of my voice and the suckle of my finger. All I could think was: If parents only knew what was happening to their babies, there is no way that they would do this. I could not continue to do this and sleep at night. I began to see what I was assisting with: forced genital cutting. I learned that I had the right to conscientiously object. I learned that there is a growing movement of people from all over the world who speak out against the cultural tradition of genital cutting in the US.
I refused to further participate in circumcisions and made it my life's work to provide parents with accurate information. This is how I repent for my hand in harming baby boys.
The information that follows is the result of three years of doctoral level study. I developed a teaching curriculum and decision making program for parents who were deciding if they wanted to circumcise their newborn son or leave him natural (otherwise known as: intact). The results of my pilot study were published in July 2015 in the Journal of Perinatal Education.
The information that follows all comes directly from medical literature & publications. The is a complete list of references following the content. In addition to the information below, this lecture from Georgetown University is a great source of accurate information: An Elephant in the Hospital
{There are drawings of penile anatomy in the information that follows}
FAQs about the foreskin and infant circumcision
· What do you think I should do?
o The decision to circumcise your son is a very personal decision. Many people feel that the decision is so personal, that it should be left up to your son himself. You will need to consider the benefits and risks of leaving your son with a natural penis and the benefits and risks of having him circumcised. This Decision Aid will help you weigh what is important to you and remind you that he can always choose circumcision for himself as an adult if he would like to be circumcised. The AAP reminds parents that circumcision is an elective procedure. Be sure that you are confident in your decision if you choose to have your son circumcised because once the foreskin is remove it cannot be put back on. (AAP, 2012; Healthwise, 2012).
· I am concerned about my son getting bullied by other boys in the locker room.
o When today’s generation of fathers were born (the 70’s thru the 90’s) circumcision was nearly universal (Herrera, Cochran, Herrera, & Wallace, 1983). Approximately half of today’s newborn boys are being circumcised and about half are remaining natural (Centers for Disease Control and Prevention, 2011). It is likely that there will be both boys with circumcised penises and boys with natural penises in your son’s locker room.
· I am concerned that my son might feel different if his penis does not look the same as his father’s penis.
o This is a very common concern, and for many Americans this is the most influential factor in the decision (Binner et al., 2002; Chantry et al., 2010; Wang et al., 2010). Regardless of if you choose circumcision or to leave his penis natural, a child’s penis and an adult’s penis look very differently, just as their noses, ears, eye color, or height may be different. Children are curious and observant. Clear and straightforward answers to his questions will help him to understand the differences.
· I have heard that babies do not feel pain. Is circumcision painful for the baby?
o It was once thought that newborns do not feel pain, but we now know that babies do indeed feel pain (AAP, 2012). The foreskin contains about 20,000 nerve endings that are the same type of nerve endings you have on the palm of your hand. The foreskin is the most sensitive part of the entire penis (Cold & Taylor, 1999; Sorrells et al., 2007) As with any surgery, circumcision is a painful procedure (Howard, Howard, & Weitzman, 1994). An injectable numbing medication is available (similar to what is used when you get a filling at the dentist) and the AAP (2012) strongly encourages that the medication be used during circumcision. The AAP (2012) states that the use of a sucrose pacifier or topical numbing cream alone is not adequate. Some providers do not use any medication to dull the pain, so you will want to ask the surgeon (or mohel) what they use for pain relief.
o Many baby boys also experience pain in the days following the procedure when they urinate and have their diaper changed. Your baby’s health care provider may recommend that you give your baby acetaminophen (Tylenol) in the first few days following the surgery. You should check with your pediatrician before giving the baby any medications.
o Adult men rarely choose circumcision for themselves, but when they do they will have access to general anesthesia that removes all the pain. Adult men also have access to much stronger pain medication during the post-operative period;just as any adult who chooses to have any cosmetic procedure, such as labiaplasty or breast augmentation.
· Is it hard to care for & clean a natural penis?
o Caring for a baby boy with a natural penis is very easy for parents. The two phrases often used to remind parents how to care for a natural penis are:
§ “Only Clean What is Seen.”
§ “When Intact, Do Not Retract.”
o At birth, the foreskin is attached to the head of the penis similarly to the way that your fingernail is attached to your nail bed. When changing his diaper or bathing him, simply wash his penis in the same way that you would wash his finger. Through the natural exploration of his body by tugging and having naturally occurring intermittent erections, his foreskin will retract in its own time. For most boys, this occurs by 3-5 years old, but for some the process is not finished until the hormones of adolescence complete the change from a child’s body into an adult’s body.
o It is important not to try to force his foreskin back. There is no need to clean under the foreskin before retraction has naturally occurred. Forced retraction causes very small abrasions (or tears) in the foreskin and glans. When these abrasions heal, it may cause the foreskin to become abnormally adhered (or stuck) to the glans (called phimosis). It will be important to tell anyone who may change him, bathe him, or perform an examination of him not to retract his foreskin.
o At the start of adolescence he can simply “retract, wash, & replace” with a soapy hand or just rinse with plain water. Males have natural lubrication and secretions, just as females do. There is no complicated care required. Parents can easily teach their sons how to clean his penis, just as they will teach him to wash under his arms, behind his ears, and brush his teeth.
o Sources: (AAP, 1984; Hayashi et al., 2011; McGregor et al., 2007; Westbrook, 1996)
· Is it hard to care for a circumcised penis?
o In the days following the circumcision, the head of his penis will be very red and sore. You will need to be very gentle during diaper changes. Depending on how the circumcision is done, you may need to dress the wound with a gauze pad and Vaseline. This will help to prevent his penis from sticking to his diaper. If the gauze pad or the diaper do stick to his penis, gently rinse with warm water to loosen the gauze pad or diaper before removing. You will notice a whitish-yellow accumulation of discharge around the site. Do not try to clean this from his penis.
o If you notice a blood clot, it is important not to wash it away or remove the blood clot. A small spot of bleeding on the gauze pad is expected, just as much as you would see after putting a bandage on a cut. However, you must call the doctor right away if the gauze pad is soaked with blood or if there is enough blood to have soaked into his diaper, rather than just a smear on the diaper surface. While the doctor is being called, wrap the head of his penis with a gauze pad and apply pressure.
o By 10 days after the circumcision, the wound should be healed. At this point, you will need to begin pushing back on the skin of his penis with each diaper change to discourage formation of adhesions (growths of skin that attach from the shaft to the head of the penis as his body attempts to re-grow his foreskin). If any skin becomes reattached, you will want to speak with your baby’s pediatrician. This may require surgical correction.
o Beyond infancy, no special care of a circumcised penis is required. Parents can easily teach their sons how to clean his penis, just as they will teach him to wash under his arms, behind his ears, and brush his teeth.
o Source: (Shelov & Altman, 2009)
· Does circumcision affect the baby’s ability to breastfeed?
o There is a lot of discussion about this topic, but not a lot of research. One randomized controlled trial from 1994 evaluated the immediate effects of circumcision on breastfeeding and found that “Infants feed less frequently and are less available for interaction after circumcision” (Howard et al., 1994, p.645). That study was not able to determine the long term effects related to continuation and duration of breastfeeding. Another study looked at only the long term outcomes and found no differences in breastfeeding duration between boys who were circumcised and boys who were not (Fergusson, Bodden, & Horwood, 2008).
· I have heard that circumcision can prevent AIDS. Can you explain that?
o Circumcision has shown a protective effect against HIV among adult men in Africa (Siegfried, Muller, Deeks, & Volmink, 2013). A Cochrane Review evaluated three randomized controlled trials conducted in Africa that showed ~40-60% decrease in adult men contracting HIV after they were circumcised versus the men who were not circumcised (Siegfried et al., 2013). It is not yet known if the results of the trials from Africa are applicable here in the U.S. (Mills et al., 2008; Sullivan et al., 2007).
o The Centers for Disease Control and Prevention (CDC, 2013) noted that there are important differences between the populations studied in Africa and the U.S. population. The HIV rate in the areas where the studies were conducted is between 6%-19% and predominantly transmitted during male/female intercourse. In the U.S., the HIV rate is 0.4% and is predominately transmitted during male/male intercourse (CDC, 2013; Sullivan et al., 2007). Based on the estimated risk reduction from the African trials and the HIV rate in the U.S., the CDC (2013) reports that 1,231 white males would need to be circumcised in order to prevent one case of HIV among this group. Heterosexually acquired HIV is rare in the U.S., except for men with high risk behaviors who account for 31% of new HIV infections (CDC, 2013). It is unclear if circumcision is protective among men who have sex with men in the U.S. (CDC, 2013).
o The theory to explain the potential link between less HIV and circumcision is that the foreskin contains immune cells to fight off infection and these are the cells that HIV targets. It is thought that these immune cells bring HIV into the body (CDC, 2013). However, this has not been proven.
o A study of 748 U.S. Navy Sailors did not find an association between circumcision and less HIV (Thomas et al., 2004).
o Both men with circumcised penises and men with natural penises can contract HIV with unsafe sex practices. Regardless of circumcision status, condoms are a very effective method of prevention for HIV & sexually transmitted infections (Mills et al., 2008; Siegfried et al., 2013; Sullivan et al., 2007; Thomas et al., 2004).
· I have heard that circumcision can prevent bladder infections. Can you explain that?
o Urinary tract infections (UTIs) are rare among both boys with a circumcised penis and boys with a natural penis. UTIs can be successfully treated with antibiotics (Healthwise, 2012).
o There is scientific evidence that boys who are circumcised have fewer UTIs than boys who are not circumcised, however the rate of complications from circumcision is calculated to be equal to or greater than the chances of having a UTI (Singh-Grewal et al., 2005). This means that boys are more likely to have a complication from circumcision than have a UTI.
o About 100-111 healthy boys will need to be circumcised in order to prevent one or two UTIs (AAP, 2012; Singh-Grewal et al., 2005). This decreased risk of UTI from circumcision is only applicable to the first year of life, beyond the first year the rates of UTI are similar (AAP, 2012; Singh-Grewal et al., 2005).
o Based on the latest review of this research, the data “[does] not support the routine circumcision of normal boys with standard risk in order to prevent UTI” (Singh-Grewal et al., 2005, p. 858). Protection from UTIs from circumcision will be of the most benefit to boys with abnormalities of the urinary tract or with recurrent infections (AAP, 2012; Singh-Grewal et al., 2005)
The Natural Penis
Anatomy
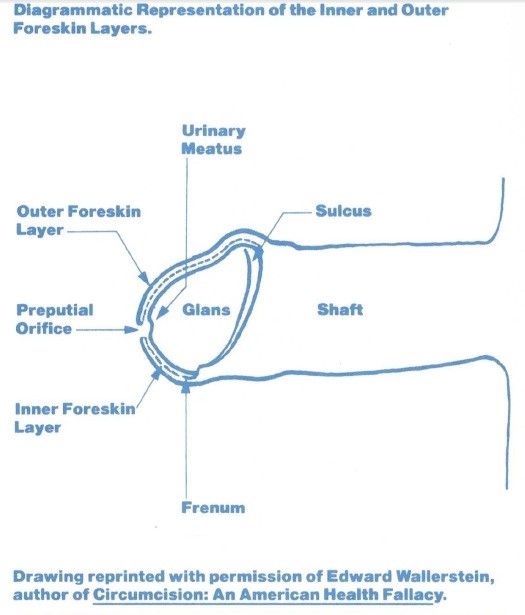
Males are born with a continuous layer of skin covering the penis. There is no distinct beginning of the foreskin when looking at the penis. The skin that covers that head of the penis (the glans) provides protection, lubrication, and sensation and is called the foreskin (or the prepuce). Both males and females have a foreskin. In females, the foreskin covers the clitoris (called the clitoral hood). From the inside of the male foreskin, there is a space about half way down the penis where the foreskin becomes a separate layer from the shaft of the penis, this space is called the sulcus. At birth, these layers are fused together and do not move or function separately. Over time, sometimes within the first few years and sometimes upon adolescence, the foreskin separates from the glans and becomes retractable to prepare for intercourse (AAP, 1984). Exposure of the glans is an adult sexual function.
The foreskin has five layers, the inner most layer is the mucousal layer (like you have inside the cheeks of your mouth and the inner layer of the labia in females). The glans of the penis has this same mucousal layer. This inner most layer of the foreskin is rich with nerve endings and Langerhan’s cells (which are immune cells that fight infection).
The layer next to the mucosal layer is the lamina propria, which is highly vascularized and responsible for blood supply to the foreskin.
The middle layer of the foreskin is the Dartos muscle. The Dartos muscle is a muscular layer that is continuous from the scrotum, down the shaft of the penis, into the forsekin, to the opening at the tip of the foreskin. The Dartos muscle allows for constriction and expansion to control for temperature changes. It allows for a tightly “puckered” foreskin opening in newborns, in order to keep out contaminants, such as urine and feces in the diaper. This puckered opening becomes looser as foreskin retraction occurs over several years.
The layer just below the skin surface is dermis, which contains larger nerve branches, connective tissue, and blood vessels. It is a highly elastic layer and allows for ease of mobility and ensures that the foreskin returns to its resting position after erection or retraction. The dermis also contains the Meissener Corpuscles, which are very sensitive nerve endings. Humans also have Meissner Corpuscles on the palm of their hands.
The outer most layer of the foreskin is the the same type of skin that is continuous with the shaft of the penis.
The frenum, or frenulum, anchors the foreskin to the ridge on the underside of the glans edge. From the frenulum, there is a band of tissue called the rigded band. This is often the most highly sensitive area for men (Cold & Taylor, 1999).
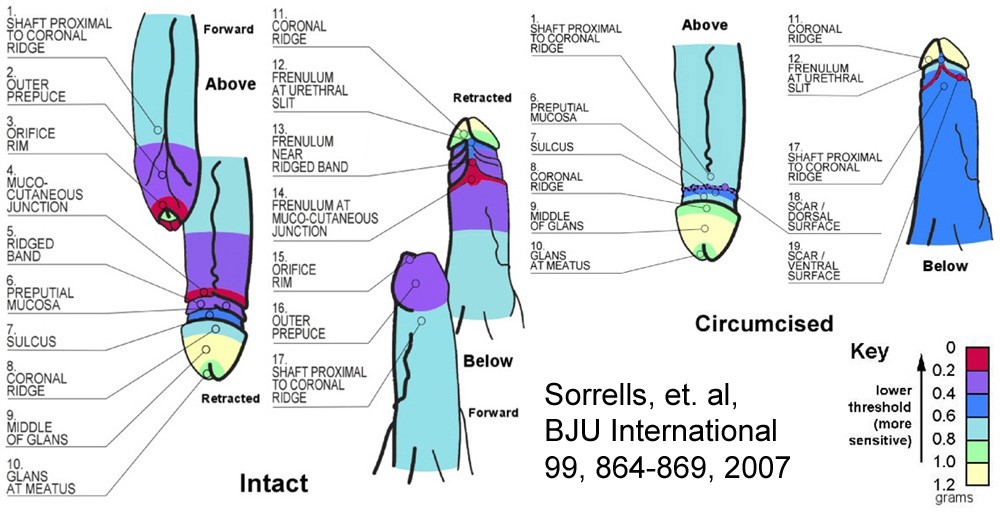
The ridged band & frenulum and the tip of the foreskin are the most sensitive areas of the penis. The remainder of the foreskin is especially sensitive, as compared to the glans. The most sensitive part of the circumcised penis is the circumcision scar (Sorrells et al., 2007).
The foreskin allows the glans to remain a sensitive and moist surface. In the absence of the foreskin to protect the mucousal glans, the glans becomes thickened (or keratinized) and less sensitive (Cold & Taylor, 1999; Sorrells et al., 2007). It also acts as a mobile sheath during intercourse. Men with natural penises contribute lubrication during intercourse and the foreskin envelops the ridge of the glans on the outwards motion. Without this enveloping, the circumcised penis withdrawals vaginal secretions with each exit contributing to abrasive intercourse and the need for artificial lubrication. Some studies have found that circumcised men and their female partners were more likely to experience sexual discomfort or difficulties as compared to men with a natural penis and their female partners (Frisch, Lindholm, & Gronbaek, 2011). The AAP (2012) does not support the claim that circumcision adversely affects sexual function or sensation.
Circumcision Procedure
Circumcisions in the U.S. are performed using 3 types of devices: Gomco, Plastibell, and Mogan Clamp. The type of device used will depend on what the surgeon prefers, and how he or she was trained. Regardless of which device is used, all circumcisions are performed in a similar fashion.
Most circumcisions performed by medical providers involve the use of a restraint board to secure the baby during the procedure. The baby’s legs are secured with velcro straps and a sterile drape is placed over the baby, with a small hole where the baby’s penis is exposed. There is usually an assistant, such as a nurse, who offers the baby a pacifier dipped in sugar water as an additional comfort measure. If the surgeon is using anesthesia, he or she will inject medication at the base of the baby’s penis to offer some pain relief. You may notice swelling or bruising where the injection was given. This is an expected side effect of an injection in the penis.
The surgeon then introduces a blunt instrument underneath the foreskin to break apart the connection between the foreskin and the glans. This is the most painful part of the procedure for the baby (Howard et al., 1994) because the innervation of these nerves are not supplied by the same nerves as are blocked by the medication injection (Cold & Taylor, 1999). Once the foreskin is separated from the glans, the surgeon makes a crimp in the foreskin in order to minimize bleeding and to judge how much foreskin to remove. A cut is made along the crimp (if using Gomco or Plastibell) and the clamp is placed.
If a Gomco is being used, a metal bell is placed over the glans to protect it from being cut. The clamp is tightened around the foreskin. The foreskin is cut by the surgeon, and the clamp is removed. The nurse or the surgeon will place a gauze bandage over the wound.
If a Plastibell is being used, a plastic ring is placed around the glans, a string is tied tightly around the foreskin against the plastic ring. The remaining foreskin is cut away. The string cuts off the blood supply to the small amount of foreskin that remains, and the remaining tissue and plastic ring will fall off in a few days. A gauze and Vaseline dressing is typically not required when using a Plastibell.
If a Mogen is being used, the foreskin will be pulled through a small slit on the metal clamp. The clamp will be tightened. The foreskin will be excised. The clamp is removed and the tissue is displaced below the glans. The nurse or the surgeon will place a gauze bandage over the wound. Source: (AAP, 2012) The manufacturers of the Mogen clamp were sued and went out of business due to repeated complaints of glans amputation or partial amputation. However, the clamp is still in use and being manufactured by other companies.
(Photo credit: http://people.howstuffworks.com/circumcision4.htm)
References
American Academy of Pediatrics (1984). Care of the uncircumcised penis [Brochure]. Elk Grove Village, IL: American Academy of Pediatrics Publications.
American Academy of Pediatrics (2012). Male circumcision. Pediatrics, 130(3), e756-e785. doi: 10.1542/peds.2012-1990
Binner, S.L., Mastrobattista, J.M., Day, M., Swaim, L.S., & Monga, M. (2002). Effect of parental education on decision-making about neonatal circumcision. Southern Medical Journal, 95(4). 457-461
Centers for Disease Control and Prevention (2011). Trends in in-hospital newborn male circumcision- United States 1999-2010. Morbidity and Mortality Report Weekly, 60, 1167-1168.
Centers for Disease Control and Prevention (2013). HIV/AIDS: Male circumcision. Retrieved from http://www.cdc.gov/hiv/prevention/research/malecircumcision/
Chantry, C.J., Byrd, R., Sage, A.C., & Calvert, E.E. (2010). Video versus traditional informed consent for neonatal circumcision. Acta Paediatrica, 99, 1418-1424. doi:10.1111/j.1651-2227.2010.01815.x
Cold, C.J. & Taylor, J.R. (1999). The prepuce. British Journal of Urology, 83(1), 34-44.
Fergusson, D.M., Boden, J.M., & Horwood, L.J. (2008). Neonatal circumcision: Effects on breastfeeding and outcomes associated with breastfeeding. Journal of Paediatrics and Child Health, 44, 44-49. doi:10.1111/j.1440-1754.2007.01202.x
Frisch, M., Lindholm, M., & Gronbaek, M. (2011). Male circumcision and sexual function in men and women: A survey-based, cross-sectional study in Denmark. International Journal of Epidemiology, 1-15. doi: 10.1093/ije/dyr104
Hayashi, Y., Kojima, Y., Mizuno, K., & Kohri, K. (2011). Prepuce: Phimosis, paraphimosis, and circumcision. The Scientific World Journal, 11, 289-301. doi: 10.1100/tsw.2011.31
Healthwise (2012). Circumcision: Should I keep my son’s penis natural? Retrieved from https://www.healthwise.net/cochranedecisionaid/Content/StdDocument.aspx?DOCHWID=aa41834
Herrera, A.J., Cochran, B., Herrera, A., & Wallace, B. (1983). Parental information and circumcision in highly motivated couples with higher education. Pediatrics, 71, 233-234
Howard, C. R., Howard, F. M., Weitzman, M. L. (1994). Acetaminophen analgesia in neonatal circumcision: The effect on pain. Pediatrics, 93 (4), 641-646.
McGregor, T.B., Pike, J.G., & Leonard, M.P. (2007). Pathologic and physiologic phimosis. Canadian Family Physician, 53, 445-448.
Mills, E., Cooper, C., Anema, A., & Guyatt, G., (2008). Male circumcision for the prevention of heterosexually acquired HIV infection: a meta-analysis of randomized controlled trials involving 11050 men. HIV Medicine, 9, 332-335. doi: 10.1111/j.1468-1293.2008.00596.x
Shelov, S.P. & Altman, T. R. (Eds.). (2009). Caring for your baby and young child: Birth to age 5 [5th ed.]. Retrieved from http://www.healthychildren.org/English/ages-stages/baby/bathing-skin-care/Pages/Caring-For-Your-Sons-Penis.aspx
Siegfried, N., Muller, M., Deeks, J.J., Volmink, J. (2013). Male circumcision for prevention of heterosexual acquisition of HIV in men (Review). Cochrane Database of Systematic Reviews, 5. doi: 10.1002/14651858.CD003362.pub2
Singh-Grewal, D., Macdessi, J., & Craig, J. (2005). Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomized trials and observational studies. Archives of Disease in Childhood 90, 853-858. doi: 10.1136/adc.2004.049353
Sorrells, M.L., Snyder, J.L., Reiss, M.D., Eden, C., Milos, M.F., Wilcox, N., & Van Howe, R.S. (2007). Fine-touch pressure thresholds in the adult penis. BJU International, 99, 864-869. doi: 10.1111/j.1464-410X.2006.06685.x
Sullivan, P.S., Kilmarx, P.H., Peterman, T.A., Taylor, A.W., Nakashima, A.K., Lamb, M.L….Mastro, T.D. (2007). Male circumcision for prevention of HIV transmission: What the new data mean for HIV prevention in the United States. PLOS Medicine, 4(7), 1162-1166.
Thomas, A.G., Bakhireva, L.N., Brodine, S.K., & Shaffer, R.A. (2004). Prevalence of circumcision and its association with HIV and sexually transmitted infections in a male U.S. Navy population (Report No. 04-10). Naval Health Research Center: Washington, D.C.
Wang, M.L., Macklin, E.L., Tracy, E., Nadel, H., & Catlin, E. A. (2010). Updated parental viewpoints on male neonatal circumcision in the United States. Clinical Pediatrics, 49(2), 130-136. doi: 10.1177/0009922809346569
Westbrook, C. (1996). What should be taught to new parents about care of their son’s uncircumcised penis? Association of Women’s Health, Obstetric, and Neonatal Nurses Voice, 4(1), 7.